Abstract
Background: Long-term complications of chimeric antigen receptor (CAR) T-cell therapy are not well-defined. Data on secondary malignancies after CAR T-cell therapy are emerging, and chemotherapy-related myeloid malignancies are of concern in these patients. We aimed to determine the incidence of myeloid neoplasms, including myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML), following CAR T-cell therapy. We also aimed to determine the prevalence of somatic mutations associated with clonal myeloid disorders such as clonal hematopoiesis of indeterminate potential (CHIP) or clonal cytopenia of undetermined significance (CCUS) in these patients.
Methods: This was a single-center retrospective cohort study that evaluated consecutive adult patients with an underlying hematologic malignancy treated with CAR T-cell therapy at our institution. We reviewed bone marrow biopsies, including cytogenetics, as well as hematologic sequencing panels following CAR T-cell therapy. Primary outcome was the cumulative incidence of myeloid neoplasms at one year. We calculated cumulative incidence with 95% confidence intervals (CI) with death as a competing event using statistical software XLSTAT.
Results: A total of 78 consecutive patients who received CAR T-cell therapy between 2016 and 2022 at our institution were included. Of these, 61.5% were male and median age at time of therapy was 65.9 years (range 21.3-85.0). Patients had received a median of 3 (IQR, 2-4.1) lines of chemotherapy prior to CAR T-cell therapy, and 30.7% had undergone a prior autologous stem cell transplant. Most common indications for CAR T-cell therapy included diffuse large B-cell lymphoma (DLBCL, 57.7%) and multiple myeloma (24.4%), with the remainder split between mantle cell lymphoma (7.7%), chronic lymphocytic lymphoma (3.8%), high-grade B-cell lymphoma (2.6%), and one patient each with follicular lymphoma, follicular lymphoma transformed to DLBCL, and primary mediastinal B-cell lymphoma. Most common CAR T-cell therapies administered were lisocabtagene maraleucel (39.7%), axicabtagene ciloleucel (24.4%), and idecabtagene vicleucel (7.7%). At 30 days post-CAR T-cell therapy, 44.9% had complete response, 29.5% had partial response, 10.3% had stable disease, and 15.4% had progressive disease. A total of 37.1% died during the follow-up period; among patients who died, overall survival was a median 161 days (IQR, 104-259).
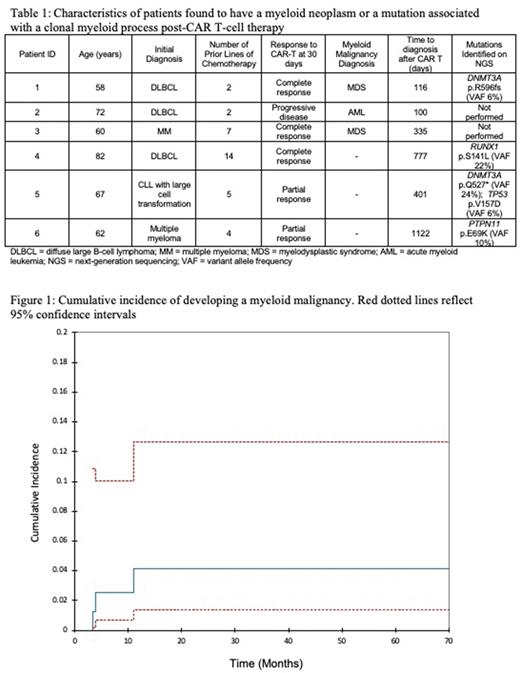
Following CAR T-cell therapy, 73.1 % of patients had a bone marrow biopsy, 10.2% had a myeloid sequencing panel, and 10.3% had a lymphoid sequencing panel from peripheral blood or bone marrow. Median time of total follow-up was 14.8 months (IQR, 6.5-28.8). Two patients developed MDS and one developed AML; characteristics of patients diagnosed with a myeloid neoplasm are shown in table 1. Cumulative incidence of subsequent myeloid neoplasms at one year was 4.2% (95% CI 1.4-12.7) as shown in Figure 1. The incidence rate for development of a myeloid neoplasm was 2.3 cases per 100 person-years (95% CI, 0.60-.7.1). Additionally, four patients, including one who developed MDS, were found to have mutations associated with myeloid disorders on hematologic sequencing; this represents 5.1% of total patients and 25.0% of those with sequencing data available. Mutations are outlined in Table 1.
Conclusion: A significant proportion of patients developed myeloid malignancies following CAR T-cell therapy, including two patients who had only received two lines of prior chemotherapy each. Mutations associated with myeloid neoplasms were found in one-quarter of the patients who had next generation sequencing performed. These findings suggest that further study is warranted to better define the causative role of CAR T-cell therapy in the development of myeloid disorders.
Disclosures
Arnason:Bristol Myers Squibb: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.